Fallen off the bike? Cesarean? Burn from the oven door?
It is common for scar tissue to form after an injury or an infection, and scars will always be present after surgery such as breast augmentation or caesarean (C-section).
Scar tissue is a natural part of the healing process and most of us have at least one place on the body where scar tissue reminds us of various life events. Some scars do not bother us, while others, such as a scar after a caesarean, can make you feel uncomfortable when wearing certain clothing. Other scars can look ugly, itch or feel tight which in turn leads to a wish of finding an easy and painless treatment method to remove the scar. Keep in mind that it is not possible to completely remove a scar, but it is possible to greatly reduce the visibility of them.
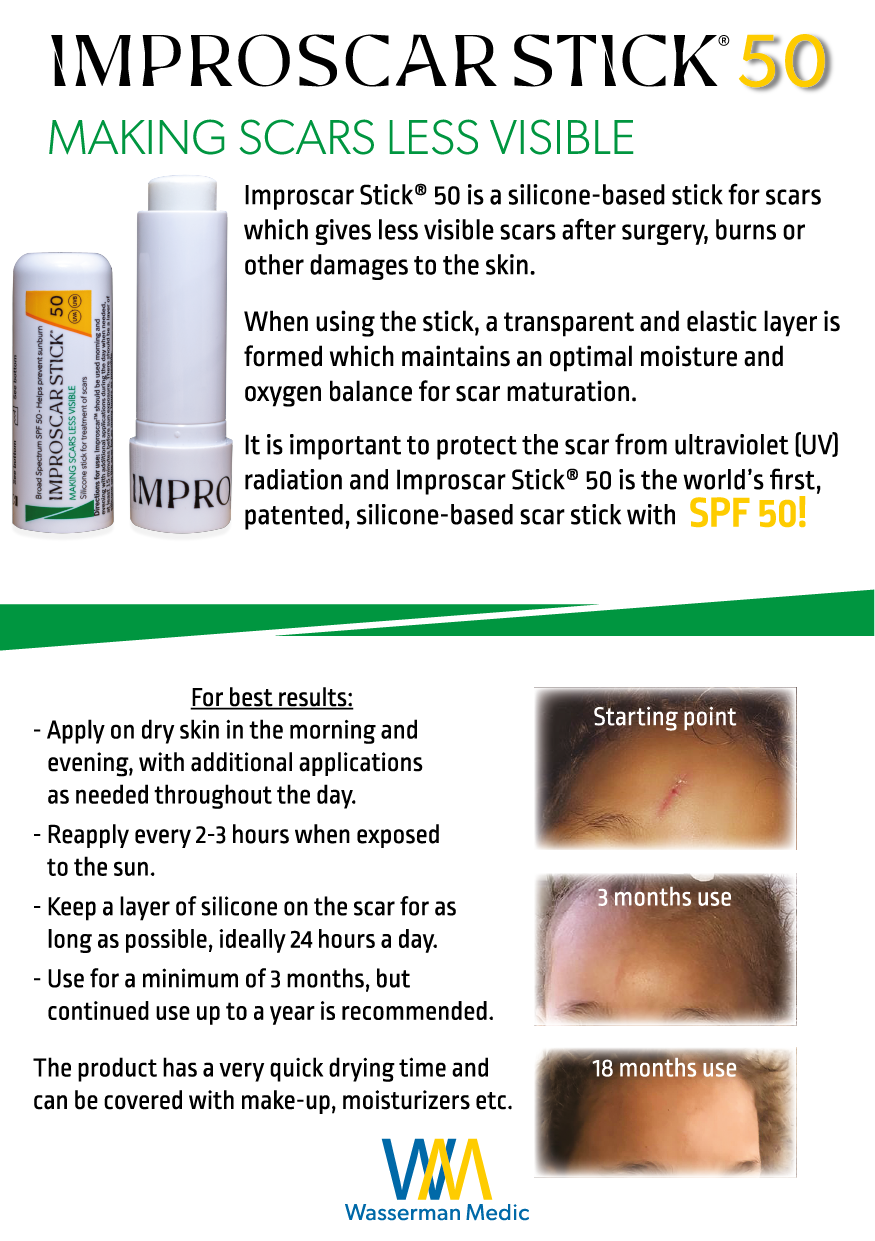
With our scar treatment products you can create a transparent and waterproof film over the scar leading to an optimal environment for scar maturation. Both Improscar Stick® and Improscar Patch™ can also protect the scar from external stresses such as rain, sweat, friction from clothes, UV radiation etc. No matter where on the body you have a scar, Wasserman Medic can assist you in reducing the visibility of it.
Our products are made with medical grade silicone. Doctors have used medical silicone products to treat scar tissue since 1982 and it has showed good results and safety documented in several studies. Our silicone sticks and silicone patches are both effective, safe and flexible.

How do scars form?
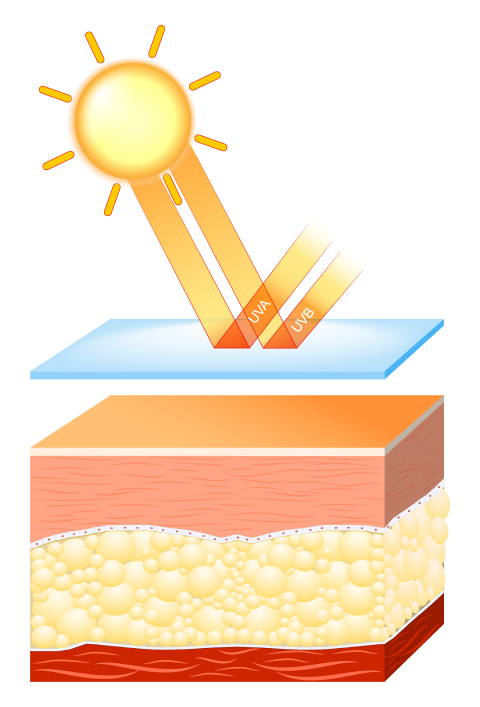
Scars are formed when the body produces fibrous tissue, e.g. collagen, to repair a wound. The new tissue differs from the original skin and is more sensitive to UV-radiation. Sweat glands and hair follicles are missing, which also makes the scar less resistant and more sensitive to temperature changes. Scar maturation takes at least a year and the scar changes from being red and perhaps itchy and hard to becoming softer and less red.
-
Sale!
Improscar Stick – Night & Day Dual Pack
€77.00Original price was: €77.00.€68.00Current price is: €68.00.
Different types of scars
Hypertrophic scar
The appearance of the scar is not always linked to the size of the initial wound but depends on a number of individual factors.
Hypertrophic scars comprise an abundance of scar tissue limited to the original wound surface. Hypertrophic scars are often red, raised and can feel tight and itchy. This type of scar usually occurs where the skin is often bent and stretched (joints for example) and is also more common in children and adolescents. Hypertrophic scars can turn into a regular linear scar with time, especially with proper scar treatment such as silicone.

Keloid
Keloids are reminiscent of hypertrophic scars but are larger because scar tissue also grows outside of the original wound surface. Sometimes the keloid is formed a long time after the injury occurred. Dark pigmented skin is more susceptible to keloid formation than light skin. Age, localization and hormonal factors can also affect the risk of a keloid forming. Teenagers and young adults have a higher collagen production and it is therefore more common for them to form keloids compared to older people. Some body parts are at higher risk of suffering from keloids such as upper torso, shoulders and the neck region. The skin is also more prone to keloid formation during a pregnancy.

How do we treat scars?
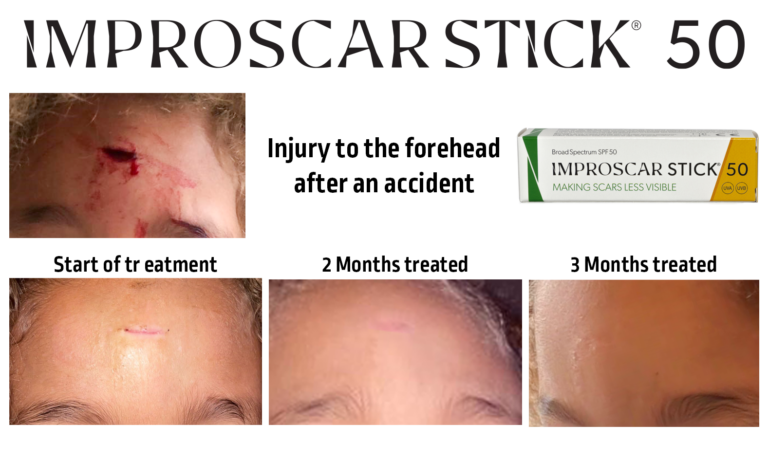
The scar forming after an injury can never be completely removed but one can make the scar less visible using the right aftercare. The first step after an injury is to make sure that the wound is cleaned and that it stays clean until it has closed. It is especially important to minimize the risk of inflammation and infection as it can otherwise exacerbate the look of the scar. Appropriate dressings can be used to accelerate the healing process and protect the wound.
General preventive scar treatment includes sun protection, softening and moisture retention. Medical silicone is considered first-line treatment for all types of scars and can be used directly after the wound has healed and new skin has formed. Since the scar needs a long time to become completely “mature” it is important to protect it from sun exposure (UV-radiation) through clothing and / or sun protection products. Otherwise, there is a risk that the scar becomes discolored. It may become darker or lighter than adjacent skin because the amount of melanin in the scar differs from “normal” skin. The scar should also be kept soft and moisturized in order to reduce the fluid loss that otherwise occurs through the scar tissue. By using products containing silicone this loss of fluid can be prevented.
In the case of major wounds, such as a larger burn, there are studies that indicate that pressure dressings can be beneficial on scar maturation. This type of dressing is often used in combination with a silicone layer to maintain skin moisture balance.
Other types of scar treatments can include laser, dermabrasion and freezing. In these treatments, medical silicone can serve as a complement to ensure optimal end results.
Recommendations on scar treatment
European guidelines on scar treatment, 2014 (1)
Linear scars caused by surgery or accidents.
Sunscreen combined with silicone treatment
Widespread hypertrophic scars caused by burn, accident or infection
Avoid sun exposure (use sunscreen)
Silicone + compression
Moisturizer, physiotherapy can help
Keloids
Avoid sun exposure (use sunscreen)
Silicone + compression
Moisturizer
For all scars, the effect of current treatment should be evaluated after 2 – 3 months.
For linear “normal” scars, the silicone treatment can continue as long as the scar responds to the treatment. Scars may need up to a year or more before it is completely inactive.
A hypertrophic scar or a keloid that does not respond to silicone treatment alone may need further treatments in combination with silicone, for example corticosteroid injections. This is decided by the physician.
Silicones for scar treatment
Medical silicones have been used since the 1980s and have a well-documented effect and safety on scar treatment (2) (3) (4) (5) (6). The silicone smoothes, softens and reduces the visibility of scars. The mechanism of action is not fully understood, but the current theory is that when silicone is applied to the skin, a water-resistant membrane is formed which protects the scar and restores the water balance. The silicone membrane permeates oxygen, which allows the skin to breathe and this is a contributing factor to keeping the scar moisturized. Silicone is a large molecule that cannot penetrate the skin and be absorbed by the body.
Medical silicone products are available in several designs, where silicone gels, silicone sticks and silicone sheets are the most common. In a comparative study between silicone sheet and silicone gel, the different treatments proved to be equally effective (7). The stick is a further development to simplify the application of the silicone. One can choose product depending on where on the body the scar is and how big it is. For smooth body surfaces that are covered with clothing, silicone sheets may be suitable. The sheet also provides protection against friction/rubbing from clothes on the scar.
To obtain the desired effect, the scar should be covered with silicone for as many hours of the day as possible. If the scar is exposed to sun, it is important to choose a silicone product that also contains sunscreen, preferably with SPF 50.
The side effects that patients have experienced during silicone treatment are linked to sheets as these can create heat rash and smelly skin (8). Some variants of sheets must be taped to be held in place. This further increases the risk of irritation to the skin. It is very rare for side effects to be reported with silicone gels or silicone sticks.



References:
1. Management of scars: updated practical guidelines and use of silicones. Meaume S, Le Pillouer-Prost A, Richert B, Roseeuw D, Vadoud J. s.l. : Eur J Dermatol, 2014, Vols. Jul-Aug;24(4):435-43.
2. A randomized, placebo-controlled, double-blind, prospective clinical trial of silicone gel in prevention of hypertrophic scar development in median sternotomy wound. Chan KY, Lau CL, Adeeb SM, Somasundaram S, Nasir-Zahari M. : Plast Reconstr Surg, 2005, Vol. Sep 15;116(4):1013-20.
3. A randomized controlled trial of hydrocolloid dressing in the treatment of hypertrophic scars and keloids. Phillips TJ, Gerstein AD, Lordan V. : Dermatol Surg, 1996, Vol. Sep;22(9):775-8.
4. Prevention of hypertrophic scars and keloids by the prophylactic use of topical silicone gel sheets following a surgical procedure in an office setting. Gold MH, Foster TD, Adair MA, Burlison K, Lewis T. : Dermatol Surg, 2001, Vol. Jul;27(7):641-4.
5. Topical Silicone Sheet Application in the Treatment of Hypertrophic Scars and Keloids. Westra I, Pham H, Niessen FB. : J Clin Aesthet Dermatol, 2016, Vol. Oct;9(10):28-35.
6. Comparison of efficacy of silicone gel, silicone gel sheeting, and topical onion extract including heparin and allantoin for the treatment of postburn hypertrophic scars. Karagoz H, Yuksel F, Ulkur E, Evinc R. : Burns, 2009, Vol. Dec;35(8):1097-103.
7. Does the form of dressings matter?: A comparison of the efficacy in the management of postoperative scars between silicone sheets and silicone gel: a randomized controlled trial. Lin YS, Ting PS, Hsu KC. : Medicine (Baltimore), 2018, Vol. Aug;97(32).
8. Prevention of postsurgical scars: comparsion of efficacy and convenience between silicone gel sheet and topical silicone gel. Kim SM, Choi JS, Lee JH, Kim YJ, Jun YJ. : J Korean Med Sci, 2014, Vol. Nov;29 Suppl 3:S249-53.